- Visibility 22 Views
- Downloads 2 Downloads
- DOI 10.18231/j.ijceo.2025.027
-
CrossMark
- Citation
A study of ocular trauma at tertiary care center hospital in Bhavnagar
Introduction
Ocular trauma is a prominent preventable cause of visual disability. In most cases, traumatic corneal or corneoscleral injuries of the eye usually lead to a drastic change in visual acuity due to the development of corneal opacities or traumatic cataracts, and in severe cases, loss of the eye due to infection and/or endophthalmitis.[1]
At least 2.2 billion individuals around the world are visually impaired. Nearly half of these instances, or at least 1 billion, could have been avoided or are still being treated. According to the WHO, there are 55 million eye injuries observed that limit everyday activities, 1.6 million of which result in blindness every day, and 7,50,000 of which necessitate hospitalisation.[2], [3]
Corneal laceration can be a partial-or full-thickness injury to the cornea. A partial-thickness injury does not violate the globe of the eye. A full-thickness injury penetrates completely through the cornea or involves the adjacent limbal or scleral area. Factors to consider include but are not limited to: depth and length of laceration, location, and degree of scarring.[2], [3] A corneal laceration is an ophthalmic emergency that can lead to profound visual impairment if adequate treatment measures are not taken to minimize severe complications. Natural wound healing may take its course with timely repair and restoration of the integrity of the corneal epithelium.
The size, type, location, and agent of an injury, as well as the amount of time that has passed since the point of injury, and whether any treatment was administered prior to primary referral, all need to be considered when evaluating a corneal laceration injury because it may call for time sensitive intervention.
Up to 90% of all eye injuries, according to the National Society for the Prevention of Blindness, are avoidable, particularly in children.[4] Domestic mishaps and workplace injuries are the most frequent open-globe injuries. Initial visual acuity, the posterior extent and length of the incision, the presence of hyphema, and the presence of vitreous prolapse are significant predictive markers for the final visual result in patients with open globe injury.[1] Clinical results also depend on the availability of qualified human resources, the provision of vitreoretinal surgery facilities, and services for corneal transplantation.[3]
Aim of the study was to evaluate the impact of various injuries on the patient's visual acuity at the time of presentation to the tertiary care hospital in Bhavnagar's ophthalmology department.
Materials and Methods
A tertiary Hospital in Bhavnagar based prospective observational study with 9-month duration.600 patients were evaluated based on following inclusion and exclusion criteria:
Inclusion criteria
All patients above 18 years of age being affected by ocular trauma to otherwise normal eye and willing to give informed consent.
Exclusion criteria
Patients who have associated sever multiple injuries.
Patient selection
After taking into consideration the inclusion and exclusion criteria, ocular traumatic eyes of affected patients who presented tertiary care hospital during study period.
Methodology
Data collection was done after ethics committee approval. We were collected Demographic data like age, occupation, address, community location, etc. and clinical data like visual acuity, finding of slit lamp examination about which structure of eye involved and any intervention like x ray orbit, ultrasonography needed will be recorded from case paper.
Statistical analysis
Data was collected, compiled and tabulated in excel sheet. Qualitative data were represented as number with percentage. Quantitative data were represented as mean with standard deviation. Statistical analysis was done by SPSS 26.0 version software (IBM, SPSS, Inc.). <0.05 value considered as a statistical significant.
Observation and Results
We enrolled 600 patients with ocular traumatic injuries who were having normal eyes previously. These patients were enrolled between December 2020 and Jun 2021 at our institute. We selected 600 patients based on exclusion as well as inclusion standards. Among 600 patients, the highest percentage observed in the age group of 19-30 age group. The lowest percentage observed in the age group of >60 years. In the age group of 31-40 years, 41-50 years, and 51-60 years, observed as following percentage: 39%, 13%, and 4.2%.72% were males whereas 28% were females observed in our study. 60.3% patients came from rural area whereas 39.7% patients came from urban area. Among 600 ocular traumatic injured patients, 53% affected with right eye, 43% affected with left eye and 4% affected with both eyes. ([Table 1])
|
|
Frequency |
Percent |
|
Bilateral |
24 |
4 |
|
Left |
258 |
43 |
|
Right |
318 |
53 |
|
Total |
600 |
100 |
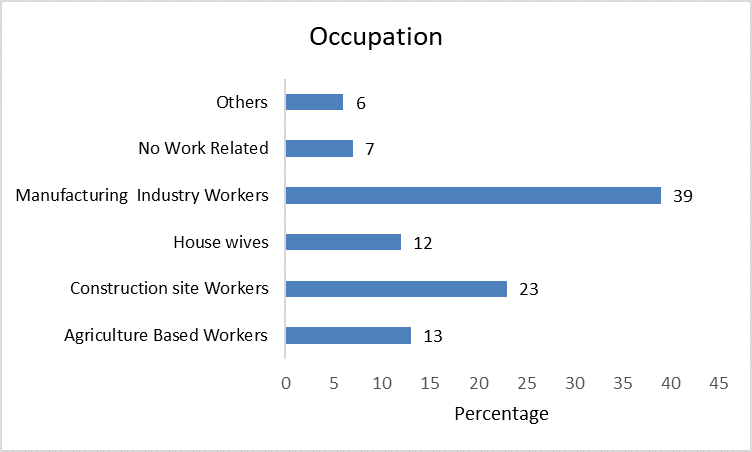
We observed that 39% were manufacturing industry workers, 23% were construction site workers, 13% were agriculture based workers, 12% were housewives, 7% injuries were not work related and 6% were due to other causes. So, manufacturing related workers more prone to affected with ocular trauma injuries observed in our study. ([Figure 1])
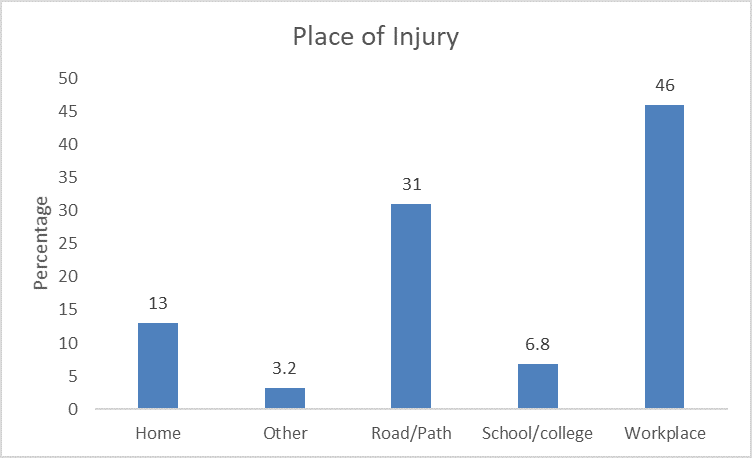
Among 600 ocular traumatic injuries patients, 31% were injured at the road area 46% were injured at workplace, 13% were injured at home, 6.8% were injured in school[Figure 2] )
We observed that 32.2% patients were injured with blunt objects, 29.2% patients were injured with sharp objects, 15.8% patients were injured due to road traffic accident, 10% patients were injured due to fall from site or other work area, 6% patients suffered burns and 6.8% patients were injured due to other objects. ([Table 2]) Among 600 ocular traumatic injuries patients, 61.2% were closed globe injuries whereas 38.8% were open globe injuries. Among 600 patients, 81% patients were not use eye protection device whereas 19% patients used eye protection device.
|
|
Frequency |
Percent |
|
Blunt object |
193 |
32.2 |
|
Sharp Object |
175 |
29.2 |
|
Fall |
60 |
10 |
|
Burn |
36 |
6 |
|
RTA |
95 |
15.8 |
|
Other |
41 |
6.8 |
|
Total |
600 |
100 |
Among 600 ocular traumatic injuries patients, highest percentage of patients injured due to accidental causes whereas least percentage of patients injured due to self-inflected injuries. ([Table 3])
|
|
Frequency |
Percent |
|
Accidental |
414 |
69 |
|
Assaulted |
152 |
25.3 |
|
Unknown |
22 |
3.7 |
|
Self-inflected |
12 |
2 |
|
Total |
600 |
100 |
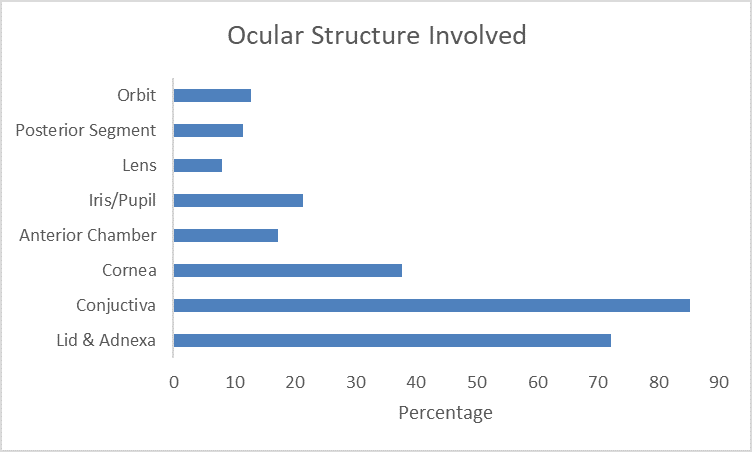
Among 600 ocular traumatic injuries patients, 72.2% were lid & adnexa, 85.3% were conjunctiva, 37.7% were cornea, 17.2% were anterior chamber, 21.3% were iris/pupil, 8% were lens, 11.5% were posterior segment, 12.8% were orbit, which are part of ocular traumatic injuries. ([Figure 3]) 61.2% were treated surgically whereas 38.8% were treated conservatively.
|
Visual Acuity at presentation |
||
|
|
Frequency |
Percent |
|
<6/60 |
283 |
47.2 |
|
≥ 6/60 -6/24 |
102 |
17 |
|
≥ 6/18 |
239 |
39.8 |
We observed that 47.2% were having visual acuity (<6/60), 17% were having visual acuity (≥ 6[Table 4])
Discussion
The phrase "ocular trauma" is used extremely broadly. It can involve any structure between eyelids up to the optic nerve, which makes gathering and processing data challenging and causes inconsistencies in the results that are ultimately produced. Therefore, for more efficient assessment and treatment, each type of injury in ocular trauma requires a specific approach. The outcomes of different studies carried out in various geographic places vary by age, gender, trauma infliction method, etc. The variances highlight the impact of various data collection techniques, socioeconomic conditions, and population industrialization on the epidemiology of eye injuries. Although ocular damage is a major source of preventable vision loss, particularly in developing countries, there has been little progress in understanding the epidemiology and prevention of eye trauma until recently. The prevalence of occupational trauma has been found to reduce when protective equipment are used, although numerous studies have revealed inadequate usage and a lack of understanding of protective eyewear.[5] Any disease prevention effort must begin with an understanding of the severity of the problem, as well as the illness's distribution and determinants. We therefore intend to conduct an observational study on ocular trauma patients who come to our tertiary care facility.
Age
In our study, 80.67% of the participants were of the youngest age group (<40 years) that was severely affected by traumatic ocular injuries. Due to their intensely motivated desire to have fun and their high risk for economic success. This age group was greatly impacted. Our findings are consistent with earlier researches done by Singh K. et al.,[6] Karve S. et al.,[7] and Kushwala R.N et al.[8] In the study by Kushwala R.N. et al.,[8] traumatic damage afflicted 64.3% of patients who were older than 35 years old. Our research is analogous to that of Karve S. et al.,[7] who found that 65.25% of people under the age of 45 had traumatic eye injuries.
Our study is consistent with that of Singh K et al.[6] According to his observation, 38.8% of study subjects were injured in the age group of <25 years, whereas in our study, 41.2% were injured in the age group of 19–30 years. Similar findings were observed in different studies related to prevalence of ocular trauma in age (<40years).
Gender
In our study, males (72%) were more severely affected by traumatic injuries compared to females (28%). So, we can say that male to female ratio was 2.57:1. Our study results were inconsistent with those of Wong et al.,[9] Singh K. et al.[6] and Kushwala R.N. et al.[8] Younger men are more likely to sustain eye injuries due to increased occupation, sports, and a risk-taking and adventure-seeking behavior.[10] This phenomenon appears to be widespread throughout the world, as shown by the prevalence of males in younger age groups reporting eye injuries in India[11] as well as other developing and developed nations.[12], [13], [14], [15], [16]
Place of occurrence of eye injuries
Workplace injuries were the commonest cause of injury, similar to studies from India and other countries.[17], [18], [19], [20] In our study, we observed that higher number of manufacture related workers and construction related workers sustained ocular injuries. Our study is consistent with the Sengupta P. et al.[21] study. In this study, the incidence of eye injuries in agriculture was found to be lower than in construction. Our study is also comparable with Singh K. et al.[6] study. In their study, it was observed that highest affected patients worked as industry worker.
We observed that highest traumatic injury occurred at work place (46%) and on the road (31%). Our study was consistent with Sengupta P. et al.[21] According to their study, 41.06% were injured at work, while 11.17% were injured at home. Singh K. et al.[6] also observed the same results. However, Kushwala et al.[8] observed that road accidents were the most common cause of ocular injury. Studies mentioned in the table given below, observed results similar to our study.
Mode of injury
According to our study, sharp objects (29.2%), road traffic accidents (15.8%), and blunt objects (32.2%) were major contributors to the cause of ocular traumatic injury. The mode of injury was affected based on age, gender, and place. Our study was comparable with the Jac-Okereke C.C. et al.[22] study. According to his observation, blunt objects affected 57%, 20% were affected by sharp objects, and 18.5% were affected by road traffic accidents. Studies mentioned in the table given below, observed results similar to our study.
Visual acuity
Visual impairment following occupation related trauma has been shown to decrease the quality of life and lead to emotional and economic disturbances in the social context. Use of protective devices has been shown to decrease the incidence of occupation related trauma but multiple studies have shown a poor use and a lack of awareness of protective eyewear.
According to our observation, 47.2% had visual acuity of <6/60, 17% had visual acuity 6/60 to 6/24 and 39.8% had visual acuity ≥6/18 after traumatic eye injury. A traumatized ocular region can sometimes cause blindness and rupture the structure of the retina. Our study is also comparable with the Alem K.D. et al.[23] They found that 68.22% had worse visual acuity, 5.30% had medium visual acuity, and 28.3% had good visual acuity. Similarity, in a study conducted in Uttrakhand India, 56.5% patients were presented with (<3/60 visual acuity). On the other hand, in a study conducted in Dhulikhel Hospital, Nepal, 83.92% patients presented with VA of better than 6/12 and only 2.67% patients under blindness category. Among traumatic injured patients, conjunctiva affected in 85.3% of cases, the lid and adnexa in 72.2%, the cornea in 37.7%. The anterior chamber affected by 17.2%.
Conclusion
This study highlights epidemiology of ocular trauma in western India. Based on this study public awareness, school awareness programme and medical officials as well as medical and nursing staff trainers should be educated about importance of eyes and basic triage management of ocular trauma. They should be motivated for utilization of services in the event of trauma irrespective of gender, age or type of injury. Mass health education and awareness about risk of ocular trauma, morbidity caused by it, and need to adopt safety equipment such as goggles, protective masks, or preventive strategies should be focused, especially during working, driving, playground, and at a school
Source of Funding
None.
Conflict of Interest
None.
References
- ALP Madhusudhan, LM Evelyn-Tai, N Zamri, H Adil, WHi Wan-Hazabbah. Open globe injury in Hospital Universiti Sains Malaysia - A 10-year review. Int J Ophthalmol 2014. [Google Scholar]
- A Adesina, MA Silverberg, FA Talavera, D Lavenburg, BE Brenner. Corneal Laceration. 2023. [Google Scholar]
- ES Saka, KF Monsudi, V Olatuji. Traumatic corneal laceration in northwestern Nigeria. J West Afr Coll Surg 2017. [Google Scholar]
- JF Salmon. . Kanski's Clinical Ophthalmology E-Book: A Systematic Approach 2019. [Google Scholar]
- LW Voon, J See, TY Wong. The epidemiology of ocular trauma in Singapore: perspective from the emergency service of a large tertiary hospital. Eye (Lond) 2001. [Google Scholar]
- K Singh, A Mutreja, M Bhattacharyya, S Dangda. Epidemiology and Implications of ocular trauma admitted to a tertiary care hospital in North India. US Ophthalmic Rev 2017. [Google Scholar]
- S Karve, A Kolte, A Alfia, H Rathi. Study of clinical profile of ocular trauma at a tertiary eye care centre. Int J Contemp Med Res 2017. [Google Scholar]
- RN Kushwaha, R Rashmi, RC Gupta, P Gupta. Profile of ocular trauma in tertiary care centre. J Evol Med Dent Sci 2013. [Google Scholar]
- TY Wong, BE Klein, R Klein. The prevalence and 5-year incidence of ocular trauma. The Beaver Dam Eye Study. Ophthalmology 2000. [Google Scholar]
- J Blackburn, EB Levitan, PA Maclennan, C Owsley, G Mcgwin. A case-crossover study of risk factors for occupational eye injuries. J Occup Environ Med 2012. [Google Scholar]
- B Thylefors. Epidemiological patterns of ocular trauma. Aust N Z J Ophthalmol 1992. [Google Scholar]
- RJ Glynn, JM Seddon, BM Berlin. The incidence of eye injuries in New England adults. Arch Ophthalmol 1960. [Google Scholar]
- P Desai, CJ Macewen, P Baines, DC Minassian. Epidemiology and implications of ocular trauma admitted to hospital in Scotland. J Epidemiol Community Health 1996. [Google Scholar]
- C Framme, J Roider. Epidemiology of open globe injuries. Klin Monbl Augenheilkd 1999. [Google Scholar]
- F Kuhn, R Morris, CD Witherspoon, K Heimann, JB Jeffers, G Treister. A standardized classification of ocular trauma. Ophthalmology 1996. [Google Scholar]
- DJ Pieramici, P Sternberg, TM Aaberg, WZ Bridges, A Capone, JA Cardillo. A system for classifying mechanical injuries of the eye (globe). The Ocular Trauma Classification Group. Am J Ophthalmol 1997. [Google Scholar]
- G Sobaci, T Akin, U Erdem, Y Uysal, S Karagül. Ocular trauma score in deadly weaponrelated open- globe injuries. Am J Ophthalmol 2006. [Google Scholar]
- ND Toit, H Mustak, C Cook. Visual outcomes in patients with open globe injuries compared to predicted outcomes using the Ocular Trauma Scoring system. Int J Ophthalmol 2015. [Google Scholar]
- . Eye and Face Protection. . [Google Scholar]
- Y Qi, FY Zhang, GH Peng, Y Zhu, GM Wan, WZ Wang. Characteristics and visual outcomes of patients hospitalized for ocular trauma in central China: 2006-2011. Int J Ophthalmol 2015. [Google Scholar]
- P Sengupta, M Mazumdar, J Gyatsho. Epidemiology of ocular trauma cases presenting to a tertiary care hospital in a rural area in West Bengal, India over a period of 2 years. IOSR J Dent Med Sci 2016. [Google Scholar]
- CC Jac-Okereke, CA Jac-Okereke, IR Ezegwui, RE Umeh. Current pattern of ocular trauma as seen in tertiary institutions in south-eastern Nigeria. BMC Ophthalmol 2021. [Google Scholar]
- KD Alem, DD Arega, ST Weldegiorgis, BG Agaje, EG Tigneh. Profile of ocular trauma in patients presenting to the department of ophthalmology at Hawassa University: Retrospective study. PLoS One 2019. [Google Scholar]
