- Visibility 38 Views
- Downloads 0 Downloads
- DOI 10.18231/j.ijceo.2025.004
-
CrossMark
- Citation
Patient pushback: Why some resist progressive addition lenses for presbyopia
Introduction
Presbyopia is an age-related condition affecting the eye's ability to concentrate on nearby objects.[1] This occurs because the lens of the eye gets less flexible with time, making it difficult to concentrate on close-up things. The major reason is a progressive loss of flexibility in the eye's lens, which makes it more difficult for the ciliary muscles to alter the shape of the lens for close vision activities.[2] While it cannot be avoided, its consequences can be efficiently handled with proper remedial actions. Symptoms may include difficulties reading tiny text, eye strain, and headaches. It's a normal feature of aging that affects almost everyone to some extent as they become older. Uncorrected presbyopia is the greatest cause of vision impairment in the globe.[3] According to worldwide estimates, 1.8 billion individuals have presbyopia. Out of these, 826 million have near vision impairment due to a lack of or insufficient vision correction.[4] The prevalence of uncorrected presbyopia among persons over 30 years varied from 28.1 to 63%.[5] Presbyopia has a negative impact on both individuals and the economy, particularly in poor and middle-income nations like India.[6]
Presbyopia treatment options include a variety of lenses, ranging from single-vision reading glasses to multifocal. Progressive lenses have grown in popularity due to their ability to give a seamless transition between close, intermediate, and distant vision, resulting in a more natural visual experience as compared to typical bifocal or trifocal lenses.[7] Progressive lenses provide a progressive shift in prescription strength over the lens surface, allowing presbyopia people to see clearly at varying distances without the obvious lines associated with bifocals or trifocals. According to research, while many presbyopia patients appreciate the practical benefits of progressive lenses, others may face initial difficulties during the adaptation phase or have special preferences for lens design and characteristics.[8] The adoption and satisfaction with progressive lenses among presbyopia patients are influenced by several factors, including optical performance, comfort, adaptation process, lifestyle considerations, and overall satisfaction with vision correction. Understanding these characteristics is critical not just for optometrists and ophthalmologists, but also for lens makers looking to improve product design and patient results.[9] Patient’s subjective experiences and impressions of progressive lenses are as important, yet they have received less attention. Patient perceptions include a wide variety of subjective sensations such as comfort while wearing, clarity of vision at various distances, ease of adaption, aesthetic considerations, and reported advantages in everyday activities like as reading, driving, and using digital devices.[10] The clarity of vision at different distances and the ease of adapting to progressive lenses are significant determinants of patient acceptance. The study aims to provide a detailed understanding of the factors influencing hesitation towards progressive lenses among presbyopia patients.
Materials and Methods
This was a descriptive, cross-sectional survey done at the department of ophthalmology sharda hospital, Greater Noida, Uttar Pradesh, India. Before beginning their involvement in the study, each subject gave their informed consent. The participants received a comprehensive explanation of the objectives, methods, possible hazards, advantages, and freedom to discontinue participation at any moment without facing any consequences. For all the patient demographics details, complete ocular and systematic history was taken. All participants went through a complete optometric examination which included an objective refraction; subjective refraction and slit lamp examination. The study utilized a semi-structured questionnaire prepared specifically for the investigation. Questionnaires were offered in the region's primary languages, English and Hindi. The faculty and specialists checked the validity and reliability of the questionnaire to ensure it covers all relevant aspects of the topic and verified that each question directly relates to the research objectives and covers the necessary content areas. The inclusion criteria include all presbyopia patients with normal general health, whether they are current spectacle wearers or non-spectacle users and have been advised to use progressive lenses, but have not yet adopted them or have discontinued their use. Exclusion criteria include individuals who are unable to provide informed consent, those younger than 40 years, individuals who have never been diagnosed with presbyopia, and participants who are already using progressive lenses without any issues. A prepared questionnaire was used to conduct interviews with each respondent. The examiner thoroughly explained the structured questionnaire before administering it to participants. Data collection was facilitated by two final year Bachelor of Optometry students from Sharda hospital. The questionnaire was divided into three sections: the respondent's demographic information, information on their present spectacles, including whether or not they used spectacles, the types of near correction, and the reasons they did not use progressive addition lenses. The data was coded, decoded, and analyzed statistically by using MS Excel and IBM SPSS 20.
Result
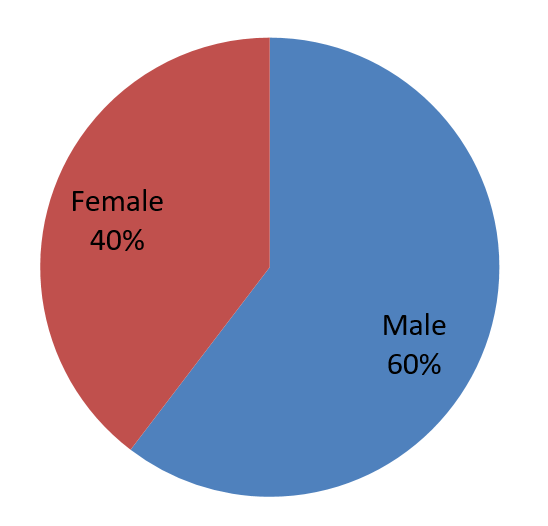
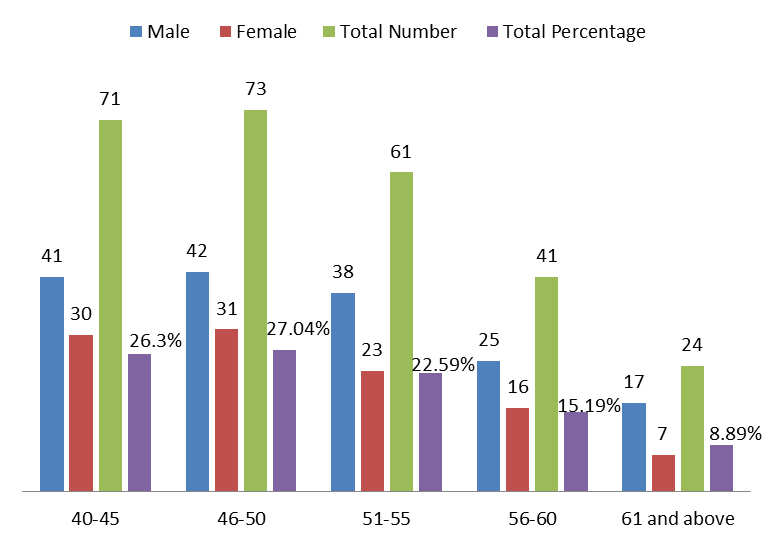
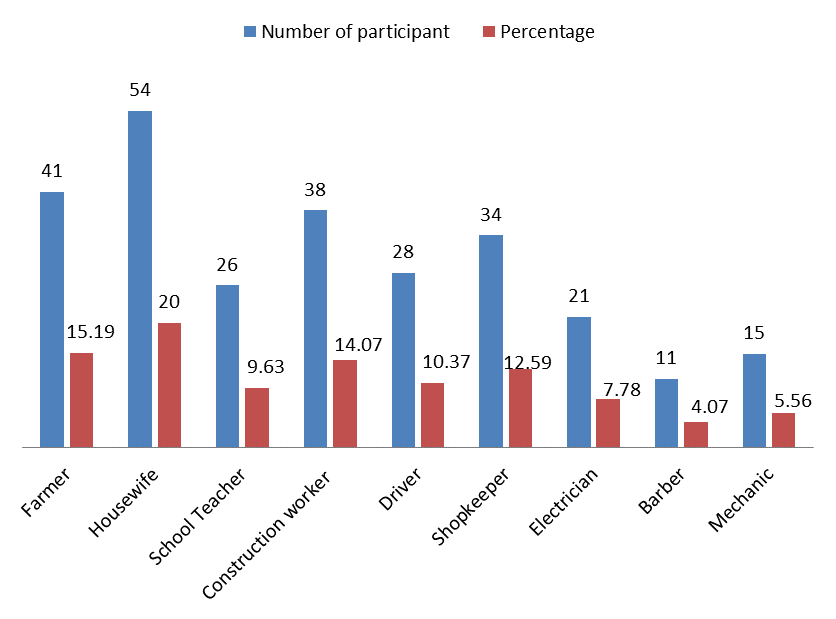
A total of 270 persons participated in this study, with 163 being male and 107 female ([Figure 1]). We discovered diverse groups of presbyopia, however the age groups of 40-45 and 46-47 had nearly same numbers of participants, 71 (26.03%) and 73 (27.05%), respectively. However, there are 24 (8.89%) fewer people in the age category of 60 and above ([Figure 2]). The study included 41 farmers, making up 15.19% of the participants. Housewives accounted for 54 participants, or 20.00%. There were 26 school teachers, comprising 9.63% of the participants. Construction workers numbered 38, representing 14.07%. Drivers made up 10.37% of the participants with 28 individuals. Shopkeepers were 34 in number, constituting 12.59% of the total. Electricians accounted for 21 participants, or 7.78%. There were 11 barbers, making up 4.07% of the participants. Mechanics made up 5.56% of the participants, with a total of 15 persons. ([Figure 3]).
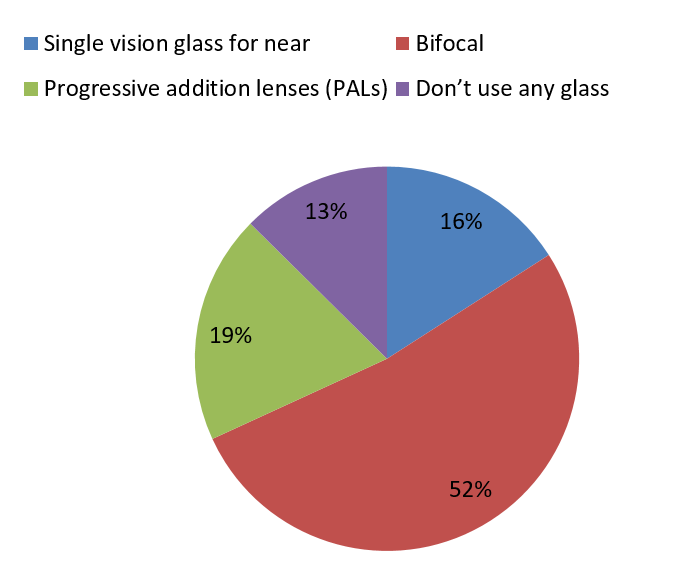
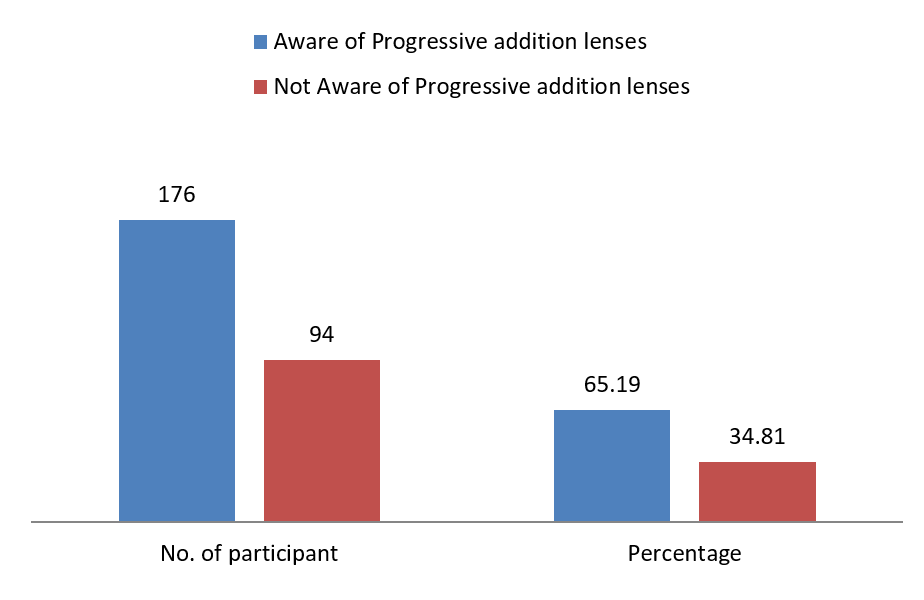
The study revealed that 43 participants, or 15.93%, used single vision glasses for near vision. Bifocals were utilized by 141 individuals, accounting for 52.22% of the total, a significant amount. Progressive addition lenses (PALs) were utilized by 52 participants, making up 19.26%. Furthermore, despite having presbyopia, 34 subjects (12.59%) did not use glasses for close vision ([Figure 4]). We found that 176 participants, or 65.19%, were aware of progressive addition lenses. In contrast, 94 participants, making up 34.81%, were not aware of progressive addition lenses ([Figure 5]).
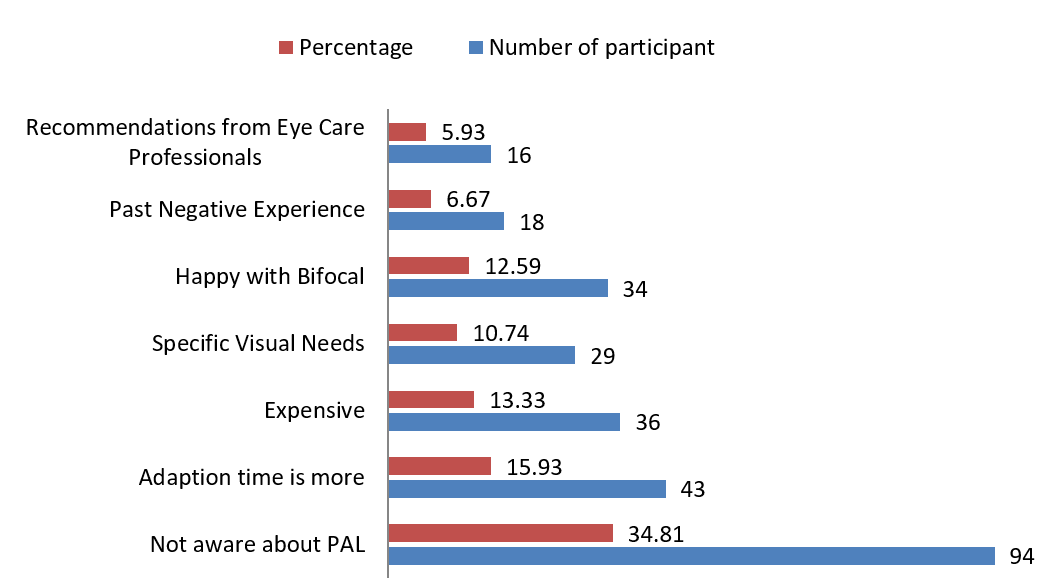
The investigation uncovered various reasons why progressive addition lenses should not be used. Out of the participants who did not use progressive addition lenses, 94 individuals (34.81%) cited lack of awareness about PALs as the reason. Additionally, 43 participants (15.93%) mentioned longer adaption times as a deterrent. Thirty-six individuals (13.33%) identified cost as a barrier to using PALs, while 29 participants (10.74%) noted specific visual needs that influenced their choice. Another 34 participants (12.59%) expressed satisfaction with bifocals, and 18 individuals (6.67%) cited past negative experiences with PALs. 16 individuals (5.93%) stated that eye care specialists' suggestions affected their decision not to utilize PALs ([Figure 6]).
Discussion
A review of presbyopia patient’s opinions of progressive addition lenses (PALs) indicates numerous critical aspects that influence their decision not to adopt this corrective option. A significant percentage of participants (34.81%) mentioned a lack of knowledge about PALs as the key reason for not utilizing them. This analysis emphasizes the crucial need for improved patient education and communication by eye care practitioners. Many patients may not be completely aware of the availability, benefits, and improvements in PAL technology. The recommendations of eye care professionals affected the choice not to utilize PALs for 16 people (5.93%). This underlines the critical role that eye care professionals play in influencing patient decisions. To provide educated and individualized recommendations, it is critical to understand each patient's lifestyle, interests, and visual demands in depth. In our study, 87.40% of presbyopia patients used some sort of near correction, which is somewhat higher than in the previous study. According to Rayan et al,[11] 58% of presbyopia patients use vision correction. This might be because the professions covered in our study require vision correction, and if they don't utilize it, their everyday activities suffer.[6] Another notable barrier observed was the extended adaption time necessary for PALs, which was noted by 43 individuals (15.93%). This conclusion is consistent with current research, which emphasizes the first problems that users frequently have while adapting to PALs,[12] such as visual distortions and the requirement for head motions to establish the optimal focus point.[13] To address these concerns, eye care specialists should provide clear instructions on what to expect throughout the adaptation phase, as well as practical solutions for an easier transition.[14]
Cost was identified as a barrier by 36 individuals (13.33%), underscoring the financial challenges associated with PALs. The previous study discovered that cost is one of the primary reasons for purchasing spectacles.[15] Progressive lenses are typically more expensive[16] than other corrective options, which can be prohibitive for some patients. This finding suggests a need for more affordable PAL options or financial assistance programs to make these lenses accessible to a broader range of patients. A remarkable 34 participants (12.59%) stated pleasure with bifocals, suggesting that classic bifocals efficiently suit some people's visual demands. The choice for bifocals might be owing to their ease, affordability, or familiarity. 6.67% of responders mentioned having previously had unfavorable encounters with PALs. According to participants, the primary reasons for discontinuing PALs include discomfort, visual distortions, eyestrain, headache, and dissatisfaction with visual quality.[17] Addressing these concerns entails identifying the individual issues faced and offering answers or alternatives that might improve their overall experience. Continuous advancements in PAL technology and personalized fitting techniques might help to dispel these unfavorable views. The previous study also indicated that people suffer discomfort, visual distortions,[18] eyestrain, headache, and using spectacles.[19] A significant 12.59% of participants were satisfied with their present bifocals, demonstrating a preference for this more traditional correction approach. Eye care specialists should undertake extensive assessments to match patients with the most effective correction alternatives, delivering individualized treatment tailored to their specific visual needs.[20] This enjoyment might be attributed to familiarity, perceived dependability, or simplicity of use. Although bifocals do not provide the same range of vision correction as PALs, they are still a feasible alternative for many individuals.
Conclusion
Presbyopia patient’s impressions of progressive lenses are multidimensional, reflecting both the benefits and drawbacks of using them. According to our findings, while many patients appreciate the smooth vision correction provided by progressive lenses, a lack of awareness and initial adaptation might be significant impediments to adoption. Individual reactions to progressive lenses underscore the importance of tailored fitting and follow-up treatment. As the population ages and the frequency of presbyopia rises, optometrists and ophthalmologists must remain up to date on advances in progressive lens technology and patient education initiatives to improve their patients visual and quality of life results.
Source of Funding
None.
Conflicts of Interest
The authors have no conflicts of interest to declare.
References
- M Millodot. . Dictionary of optometry and vision science 2017. [Google Scholar]
- SA Strenk, LM Strenk, JF Koretz. The mechanism of presbyopia. Prog Retin Eye Res 2005. [Google Scholar]
- R Bourne, JD Steinmetz, S Flaxman, PS Briant, HR Taylor, S Resnikoff. Trends in prevalence of blindness and distance and near vision impairment over 30 years: an analysis for the Global Burden of Disease Study. Lancet Glob Health 2021. [Google Scholar]
- TR Fricke, N Tahhan, S Resnikoff, E Papas, A Burnett, SM Ho. Global prevalence of presbyopia and vision impairment from uncorrected presbyopia: systematic review, meta-analysis, and modelling. Ophthalmology 2018. [Google Scholar]
- S Marmamula, S Narsaiah, K Shekhar, RC Khanna. Presbyopia, spectacles use and spectacle correction coverage for near vision among cloth weaving communities in Prakasam district in South India. Ophthalmic Physiol Opt 2013. [Google Scholar]
- I Patel, B Munoz, AG Burke, A Kayongoya, W Mchiwa, AW Schwarzwalder. Impact of presbyopia on quality of life in a rural African setting. Ophthalmology 2006. [Google Scholar]
- JL Preston. Progressive addition spectacle lenses: design preferences and head movements while reading [Doctoral dissertation]. 1998. [Google Scholar]
- CM Sullivan, CW Fowlert. Investigation of progressive addition lens patient tolerance to dispensing anomalies. Ophthalmic Physiol Opt 1990. [Google Scholar]
- . Ophthalmic Lens Technical Reference & Transmission Data. 2018. [Google Scholar]
- E Odjimogho, S Odjimogho. Survey on problems associated with the use of progressive addition lenses (pal). J Niger Optom Assoc 2004. [Google Scholar]
- REK Man, EK Fenwick, C Sabanayagam, LJ Li, P Gupta, YC Tham. Prevalence, Correlates, and Impact of Uncorrected Presbyopia in a Multiethnic Asian Population. Am J Ophthalmol 2016. [Google Scholar]
- JB Shim, HS Shim. Analysis of Adaptation for The first-time Progressive Lenses Glasses Wearers. J Korean Ophthal Opt Soc 2011. [Google Scholar]
- NAA Najmee, NH Buari, R Mujari, MI Rahman. Satisfaction level of progressive additional lens (PAL) wearers. Environ Behav Proc 2017. [Google Scholar]
- D Meister. The Optics of Free-Form Progressive Lenses. 2008. [Google Scholar]
- AA Ayanniyi, FG Adepoju, RO Ayanniyi, RE Morgan. Challenges, attitudes and practices of the spectacle wearers in a resource-limited economy. Middle East Afr J Ophthalmol 2010. [Google Scholar]
- G Savio, G Concheri, R Meneghello. Progressive lens design by discrete shape modelling techniques. Int J Interact Des Manuf 2013. [Google Scholar]
- Y Han, KJ Ciuffreda, A Selenow, SR Ali. Dynamic interactions of eye and head movements when reading with single-vision and progressive lenses in a simulated computer-based environment. Invest Ophthalmol Vis Sci 2003. [Google Scholar]
- F Benyó, L István, H Kiss, A Gyenes, G Erdei, É Juhász. Assessment of Visual Quality Improvement as a Result of Spectacle Personalization. Life (Basel) 2023. [Google Scholar]
- NAA Najmee, NH Buari, R Mujari, MI Rahman. Quality of vision of presbyopic via progressive additional lens (PALs). Asian J Qual Life 2018. [Google Scholar]
- J Dermott. Modern management of presbyopia. 2022. [Google Scholar]
